Author: Denis Avetisyan
Current heart transplant policies can be gamed, and new research argues that machine learning must account for strategic behavior to ensure fair and efficient organ distribution.
Machine learning for heart transplant allocation policy must incorporate incentive design and game theory to address strategic behavior by stakeholders.
While machine learning offers promising avenues for optimizing the allocation of scarce donor organs, current approaches often overlook the strategic behaviors of involved parties. In their position paper, ‘Position: Machine Learning for Heart Transplant Allocation Policy Optimization Should Account for Incentives’, the authors argue that successful allocation policies must explicitly address incentive misalignments across transplant centers, clinicians, and regulators. They demonstrate that overlooking these incentives can lead to adverse outcomes in US adult heart transplant allocation, necessitating a shift towards incentive-aware machine learning and mechanism design. Can integrating principles from game theory, causal inference, and social choice unlock more robust, efficient, and equitable organ allocation systems?
The Fragile Equilibrium: Balancing Scarcity and Need in Organ Allocation
The allocation of life-saving organs represents a profoundly complex challenge, perpetually strained by a critical scarcity that directly impacts patient survival rates. Demand consistently outstrips supply, forcing clinicians and policymakers to navigate intricate ethical dilemmas regarding fair and effective distribution. Each decision carries immense weight, balancing medical urgency, patient characteristics, and logistical constraints-all while acknowledging the tragic reality that not everyone will receive the organ they desperately need. This scarcity isn’t merely a numbers game; it necessitates difficult conversations about defining medical need, prioritizing certain conditions, and ensuring equitable access across diverse populations, creating a system where every allocation represents both a triumph and a heartbreaking compromise.
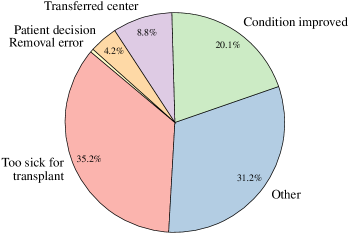
The established protocols governing organ allocation, often relying on fixed rules and predetermined criteria, demonstrably falter when confronted with the dynamic realities of organ availability and patient need. These systems, while intending fairness, inadvertently create incentives for strategic behavior amongst medical professionals and patients alike – for example, prioritizing patients deemed more likely to benefit, or manipulating listing status to improve perceived urgency. This rigidity prevents effective response to sudden shifts in donor demographics, disease outbreaks, or regional disparities in access, hindering optimal organ utilization. Consequently, the very rules designed to ensure equitable distribution can, paradoxically, contribute to inefficiencies and exacerbate inequities, prompting a search for more adaptable and responsive allocation models.
The structure of organ allocation, despite aiming for fairness, unintentionally fosters strategic behavior that can disadvantage vulnerable patients. Existing systems, often reliant on rigid criteria and geographically defined networks, present loopholes susceptible to manipulation – for instance, listing patients at multiple centers to increase visibility or selectively accepting recipients based on factors beyond medical urgency. This isn’t necessarily malicious intent, but a rational response to scarcity within the rules; however, it systematically benefits those with greater resources, social capital, or access to specialized care. Consequently, inequities embedded within the broader healthcare system are amplified, meaning individuals from marginalized communities or with limited financial means face further barriers to receiving life-saving transplants, despite potentially being equally or more deserving based on medical need.
Data-Driven Refinement: Towards a More Responsive Allocation System
Data-driven optimization in organ allocation leverages the increasing availability of comprehensive patient and organ data to move beyond traditional, often subjective, allocation rules. This approach utilizes statistical analysis and computational modeling to identify patterns and predict post-transplant outcomes, such as graft survival and patient lifespan. By quantifying the impact of various recipient and donor characteristics – including age, medical history, and immunological factors – allocation algorithms can be refined to maximize the overall benefit derived from a limited supply of organs. This contrasts with systems relying on fixed priority scores, potentially leading to more efficient matching and improved long-term outcomes for both recipients and the broader transplant population.
Machine learning algorithms applied to organ allocation utilize historical and real-time data – including donor characteristics, recipient medical information, waiting list times, and post-transplant outcomes – to predict transplant success rates and identify optimal recipient-donor matches. These algorithms, employing techniques such as regression, classification, and survival analysis, can assess the probability of graft survival and patient longevity under various allocation scenarios. By iteratively analyzing these predictions against actual outcomes, the allocation criteria can be refined to maximize the number of successful transplants and improve overall patient survival rates, moving beyond static rule-based systems to a more dynamic and responsive approach. The scale of data required necessitates robust data infrastructure and standardized data collection protocols to ensure accuracy and minimize bias in the predictive models.
Exclusive reliance on data-driven metrics in organ allocation systems introduces the risk of Goodhart’s Law, where observed figures become the targets of manipulation rather than reflecting genuine improvements in patient outcomes. Specifically, if a metric such as “time to transplant” is prioritized, hospitals may incentivize behaviors that artificially reduce this number – for example, by selectively listing healthier patients – without actually increasing the overall number of successful transplants or improving long-term survival rates. This can lead to a distortion of true performance indicators, creating a system optimized for the reported metric rather than for maximizing patient benefit and equitable access to organs. Careful consideration must therefore be given to the potential for unintended consequences when selecting and implementing data-driven optimization strategies.
Effective organ allocation systems require mechanisms that counteract strategic behavior by both recipients and providers. Incentive alignment involves structuring the system such that maximizing individual utility-such as transplant center volume or patient survival rates-coincides with the overall goal of equitable access and efficient organ utilization. This necessitates careful consideration of reporting metrics; easily manipulated indicators will be targeted, leading to inflated performance figures that do not reflect genuine improvements in patient outcomes. Strategies include incorporating independent verification of data, implementing penalties for falsification, and utilizing multi-criteria evaluation frameworks that assess performance across a broad range of indicators, thereby increasing the cost of manipulation and promoting honest reporting. Furthermore, transparent and publicly available data on allocation decisions and outcomes is crucial for accountability and to facilitate identification of potential biases or unintended consequences.
The Perils of Strategic Behavior and the Necessity of Alignment
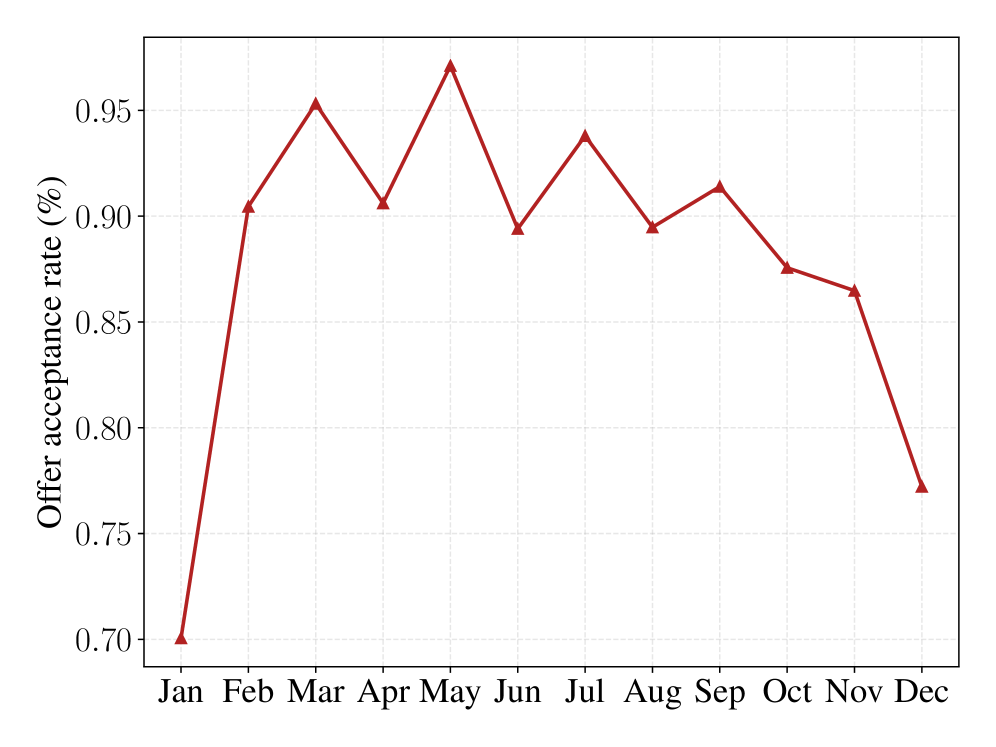
The application of medical devices, specifically intra-aortic balloon pumps (IABPs) and left ventricular assist devices (LVADs), can impact a patient’s status within organ allocation systems. Following alterations to policy, IABP utilization in cardiac patients increased significantly, rising from 7.0% to 24.9%. This increase suggests a strategic response by clinicians to improve patient priority scores, effectively creating incentives to classify patients as being in more critical condition than they might otherwise be, and thus increasing their chances of receiving a transplant. This phenomenon demonstrates how interventions can be used to manipulate a patient’s position within the allocation system, rather than solely addressing underlying physiological needs.
Strategic classification within organ allocation systems refers to the manipulation of patient characteristics reported to the allocation algorithm to improve their priority score. This behavior demonstrates how agents – including medical professionals and patients – can influence their position on the waiting list by selectively emphasizing or de-emphasizing certain features. Such manipulation isn’t necessarily fraudulent; it reflects rational responses to the incentives embedded within the allocation rules. The practice can involve optimizing reported data to fall within favorable scoring thresholds, potentially impacting the equitable distribution of organs and creating disparities in access to transplantation.
Patient behaviors such as multi-listing at multiple transplant centers and pursuing transplant tourism indicate active attempts to circumvent established allocation protocols. Data demonstrates a statistically significant difference in transplant rates between patients listed at multiple centers versus those listed at only one; multi-listed candidates achieved a transplant rate of 80.44% compared to 73.06% for those not multi-listed. This disparity suggests that accessing a broader network of transplant programs increases a patient’s likelihood of receiving an organ, driving the practice despite potential systemic inequities or increased patient burden.
Kidney exchange programs represent a successful model of incentive alignment within the organ transplantation system. These programs facilitate transplants by pairing incompatible donor-recipient pairs with other such pairs, enabling reciprocal transplants that would otherwise be impossible. This process benefits both donors, who can altruistically contribute to saving a life, and recipients, who gain access to a compatible kidney and avoid prolonged waitlist times. Data indicates that participation in kidney exchange significantly increases the likelihood of receiving a transplant for previously incompatible patients, demonstrating a mutually beneficial outcome driven by aligned incentives for both donor and recipient populations.
Continuous Evaluation and the Pursuit of a Just System
Rigorous performance monitoring, spearheaded by organizations such as the Scientific Registry of Transplant Recipients (SRTR), forms the bedrock of a continuously improving organ transplantation system. SRTR analyzes comprehensive data on transplant center outcomes – including graft survival, patient survival, and waitlist mortality – to objectively assess center performance and identify areas requiring focused intervention. This data-driven approach allows for the benchmarking of best practices, the dissemination of quality improvement strategies, and the implementation of targeted feedback mechanisms. Beyond simply identifying underperforming centers, SRTR’s analyses illuminate systemic challenges and contribute to the refinement of allocation policies, ultimately striving to maximize the benefit of this scarce resource for all patients in need.
The practice of allocating organs outside of the standard sequencing system, known as out-of-sequence allocation, is gaining prominence as a potential strategy to improve transplant outcomes, but demands rigorous oversight. Recent data indicates a substantial increase in this practice, particularly for kidney allocations, which jumped from 2% to 18% in 2023. Overall, nearly one in five organ allocations (19%) now occurs out of sequence. While this flexibility can address unique patient needs or logistical challenges, successful implementation hinges on close coordination between transplant centers and Organ Procurement Organizations (OPOs) to ensure fairness, transparency, and prevent any compromise to the overall integrity of the allocation system. Continued monitoring and evaluation of these allocations are critical to understand their impact on waitlist mortality and long-term graft survival.
Determining the optimal criteria for organ allocation necessitates a deep understanding of the values held by all stakeholders – patients, medical professionals, ethicists, and the public. Preference elicitation techniques, such as the Analytic Hierarchy Process (AHP), offer a structured approach to quantify these often-complex and conflicting values. AHP breaks down the allocation problem into a hierarchy of criteria and allows stakeholders to make pairwise comparisons, indicating the relative importance of each factor – for instance, medical urgency versus time on the waitlist, or potential benefit versus age. Through mathematical analysis of these comparisons, AHP generates weighted scores for each criterion, providing a transparent and defensible basis for refining allocation policies and ensuring they genuinely reflect societal priorities. This process moves beyond simply asking stakeholders what they want, and instead reveals the relative trade-offs they are willing to make, ultimately leading to a more equitable and effective system.
The pursuit of a just and effective organ allocation system is fundamentally hampered by conflicting incentives, a challenge that directly impacts patient survival. Current data reveal a sobering reality: 14% of patients awaiting transplantation die within the first week, underscoring the urgency of the situation. While the median time to receiving a transplant is 26 days, this precedes the median time to death on the waitlist by just 10 days, suggesting a narrow window of opportunity for intervention. This proximity highlights how seemingly small adjustments to allocation policies, or improvements in organ preservation and matching, could significantly alter outcomes for those most critically ill, yet systemic issues continue to prioritize efficiency and equitable distribution alongside immediate patient need, creating a complex landscape where aligning the incentives of all stakeholders remains the central, and most pressing, hurdle.
The pursuit of equitable organ allocation, as detailed in the paper, highlights a fundamental challenge: anticipating and mitigating strategic behavior. The system’s structure profoundly influences its outcomes, a point elegantly captured by Blaise Pascal: “The eloquence of the tongue does not persuade the heart, but the heart persuades the tongue.” This resonates deeply with the paper’s argument that a seemingly objective allocation policy can be undermined if incentives aren’t carefully considered. A ‘clever’ algorithm, devoid of awareness regarding stakeholder motivations, risks being fragile, ultimately failing to achieve its intended goals of fairness and efficiency. Simplicity in design, coupled with a holistic understanding of the system’s dynamics, remains paramount.
Beyond the Algorithm
The pursuit of optimized organ allocation, as this work highlights, too often resembles tinkering with a single valve in a complex circulatory system. One can adjust the flow, certainly, but without a thorough understanding of the entire network-the motivations, the pressures, the strategic responses of all involved-the intervention may well exacerbate existing blockages elsewhere. The application of machine learning, while promising, is not a panacea; it is merely a more sophisticated tool for mapping the currents. It cannot, of itself, create a healthy system.
Future efforts must move beyond simply predicting outcomes based on historical data. The core challenge lies in anticipating how rational actors will react to the allocation rules. A truly robust system requires incorporating game-theoretic principles-mechanism design-to actively shape incentives and align the interests of transplant centers, physicians, and, most importantly, patients. Ignoring this dynamic is akin to designing a bridge without accounting for wind resistance.
The field should also explore the limits of optimization itself. Is maximizing the number of transplants always the paramount goal? Or should considerations of long-term graft survival, patient quality of life, and equitable access-metrics far more difficult to quantify-receive equal weight? The algorithm can refine the process, but it is humanity that must define the values.
Original article: https://arxiv.org/pdf/2602.04990.pdf
Contact the author: https://www.linkedin.com/in/avetisyan/
See also:
- Gold Rate Forecast
- Top 15 Insanely Popular Android Games
- EUR UAH PREDICTION
- 4 Reasons to Buy Interactive Brokers Stock Like There’s No Tomorrow
- Did Alan Cumming Reveal Comic-Accurate Costume for AVENGERS: DOOMSDAY?
- Silver Rate Forecast
- DOT PREDICTION. DOT cryptocurrency
- ELESTRALS AWAKENED Blends Mythology and POKÉMON (Exclusive Look)
- Core Scientific’s Merger Meltdown: A Gogolian Tale
- New ‘Donkey Kong’ Movie Reportedly in the Works with Possible Release Date
2026-02-07 00:37